2022%20Pillar%20Page_Body%20Ache/Relieve%20Plantar%20Fasciitis.jpg?width=1200&name=Relieve%20Plantar%20Fasciitis.jpg)
Shelly is a busy business executive who often works in the company's overseas factories and participates in international exhibitions and conferences. During a business trip, she was about to start a busy day when she felt pain in her feet upon getting out of bed. Trying to ignore the pain, she stood up, jumped a few steps on one foot, and the pain disappeared all of a sudden.
A few hours into her day, she's standing in high heels and presiding over a meeting. Her toes were uncomfortable the entire time, which caused her feet to swell.
Whenever Shelly’s feet hurt the following days, she never thought to see a doctor or take pain medication. Even so, her feet were still so painful in the mornings that she couldn’t touch the ground. After two days of this experience, her feet felt better and healed without medicine. Do you or the people around you have a similar experience?
Plantar fasciitis and big toe valgus are common foot problems, with different symptoms and different remedies.
The differences between Plantar Fasciitis and Bunions
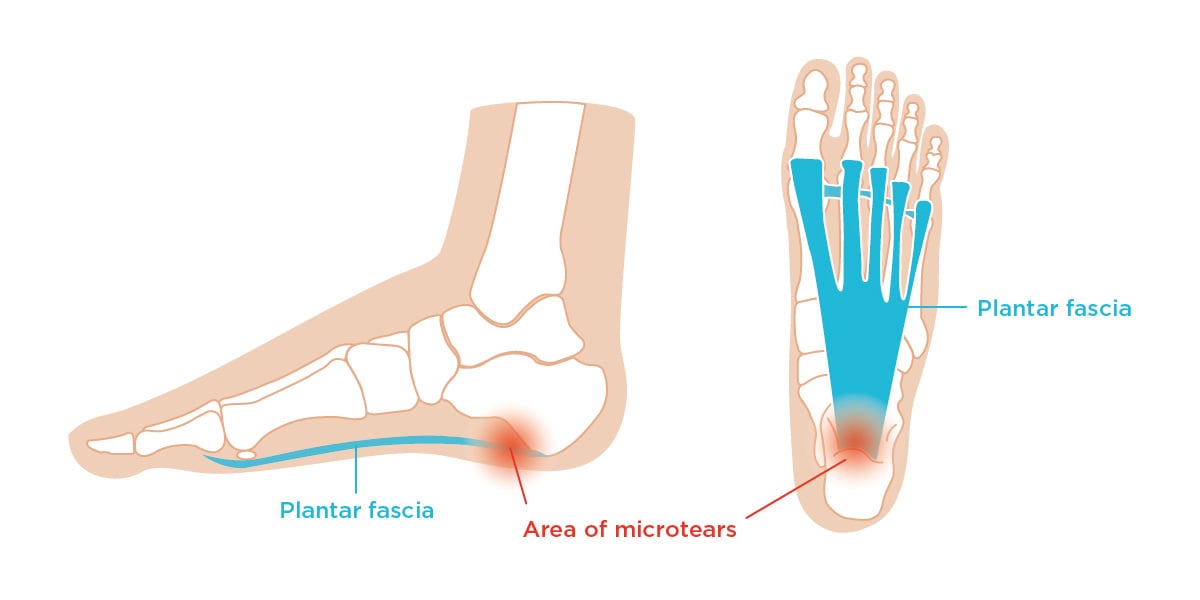
The plantar fascia connects our heel bones to the bases of our toes.
In light of this, the plantar fascia experiences a lot of wear and tear everyday whether we are aware of it or not. When we place too much pressure on this part of our body, we are more likely to damage or injure it; and when we start to experience pain in this ligament, the phenomenon is called plantar fasciitis.
No one is exempt from this condition. According to the Oxford University Hospitals, one in every ten adults experience plantar fasciitis.
Here are people who are more prone to damage their plantar fascia:
- Adults between 40 to 70, especially women, due to the gradual deterioration of their bones and ligaments. Among the aging people with plantar fasciitis, the bony spur on their heel bone can be discovered, resulting in pain and inflammation due to repeated stimulation.
- Pregnant women, due to rapid weight gain and bodily changes.
- People who are experiencing obesity or weight gain, due to the increased pressure on the ligament.
- Athletes, especially those who run long distances or do speed or hill training. Running on asphalt or concrete is also a contributing factor. Military recruits are also candidates.
- Restaurant servers, factory workers, and other laborers who need to walk around a lot.
- People with very high arches or very flat feet.
- People with tight Achilles tendons, which are the tendons connecting your heel muscles to your calves.
- People who wear shoes with soft soles or poor arch support.
However, here is a different scenario. Imagine wearing ill-fitting shoes for an office job and experiencing pain on the side of your big toe from time to time. While you decide to ignore it, the pain increases over time and soon makes walking an uncomfortable experience.
Bunions, a bony bump that forms on the base of your big toe, may seem harmless. After all, it only looks like a red, calloused bump on the outside. However, when left untreated, these can negatively affect your health.
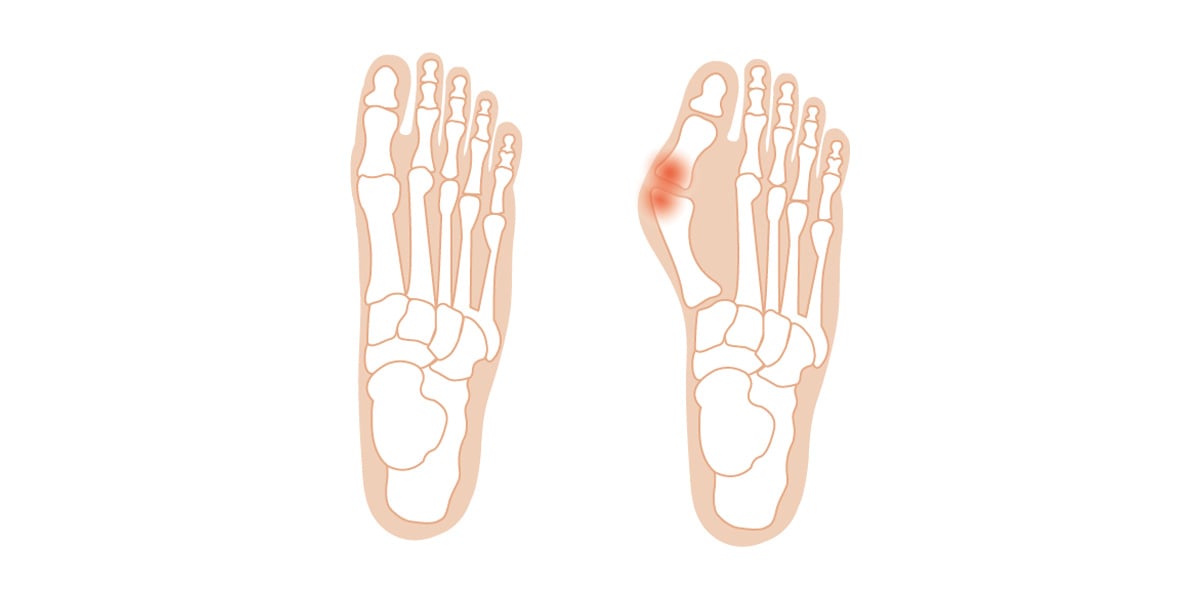
Bunions, a bony bump that forms on the base of your big toe. The valgus angle is calculated between the angle of 1st metatarsal bone and proximal toe bone. The normal valgus angle is 0- 15 degrees.
Whenever we wear smaller-sized shoes or narrower ball width shoes or are genetically prone to have arthritis, our big toe starts pointing towards our second toe, and the shape of our feet changes. Sometimes, bunions are an inherited trait from our family tree.
As both plantar fasciitis and bunions are foot-related problems, it goes without saying that the way we treat our feet is important. According to Podiatry Associates, P.C., people who wear high heels are more likely to experience these conditions. While wearing heels, our Achilles Tendon tightens, never allowing our plantar fascia a chance to relax. As high heels and stilettos tend to be narrower than other shoes, our toes are also tensed. While they may look pleasing to the eye, it is actually recommended that we do not wear heels for an extended period of time and switch them for lower heels instead. This gives our feet a chance to rest.
When to see a doctor: Plantar Fasciitis vs. Bunions
While pain is a common indicator that something is wrong with your body, it’s important to note where the pain is coming from.
When checking if you have plantar fasciitis, take note if you feel pain on the underside of your foot, particularly your heel or arch. The pain will be more noticeable when you start walking after waking up and getting out of bed. You will also notice that the arch of your foot or heel pain might feel better after walking around, but will begin hurting after standing up again after you have rested. Once you feel sharp pain on your heel after walking or standing for a long time, it’s time to book an appointment with your doctor.
Some people might try to remedy the situation by changing the way they walk (e.g. shifting their weight elsewhere), but this might actually cause other foot, knee, hip, or back problems.
During your appointment, the podiatrist will try to rule out other possible issues such as a stress fracture or a pinched nerve. The doctor might also ask you to recall your health history and injuries, list down your symptoms, and describe your daily activities. The podiatrist will do a physical assessment to understand your conditions. And go through an x-ray or an MRI, if necessary. Your podiatrist will usually recommend an ultrasound, x-ray, or MRI to see your foot anatomy. He or she may also ask you to walk around to check if your bunion has negatively affected your balance. Blood tests may also be done to rule out other issues such as gout or rheumatoid arthritis.
Though bunion and plantar fasciitis are common foot problems and sometimes they occur together, pay attention to physical symptoms, as well. Check your toe if it is red or swollen. Aside from experiencing pain under the ball of your foot, move your toes around and see if your joints are painful. Also, make sure to note if the skin over your bunion gets red or blistered from rubbing against the inside of your shoes.
How the treatment works: Plantar Fasciitis
Treating plantar fasciitis has more to do with a lifestyle change than taking painkillers and steroids. According to Orthopedics New England, 90% of patients complete their recovery in just six months after regular treatment. Here are some of them:
1. Looking for better shoes.
If you are experiencing pain, try to wear more comfortable shoes, instead. Avoid wearing leather shoes or high-heel shoes. If you are required to wear formal shoes, prepare a pair of comfortable shoes to change into once you can.
It’s important to remember that not all shoes are going to fit how our feet are built. When looking for the right kind of shoe, it needs to support your plantar fascia properly, absorb shock properly each time you take a step, and prevent you from over-pronation or supination. Combining this with #4, you will learn how to walk properly and where to place your weight when making a step.
2. Resting your feet.
As with other orthopedic problems, it is not advised for people with plantar fasciitis to stay seated or standing for too long.
If you are an athlete, try looking for more suitable training shoes that fit your build. Also, consider if you need the intervention of orthotics. Avoid hard surfaces that will strain your plantar fascia further, and adjust your training program according to your physical wellbeing.
For office workers, this may mean looking for better, custom-made shoes and switching to low-heeled shoes. Try drawing circles with your toes underneath your table. This movement can reduce the tightness of your calves, and also improve blood circulation.
3. Stretching and strengthening your ligaments and muscles.
Plantar fasciitis is often caused by restrictions within your muscle tissues. Encourage your muscles, ligaments, and tendons to grow more flexible by performing stretches. As the end goal is to make walking more comfortable for you, make sure to consistently stretch every day.
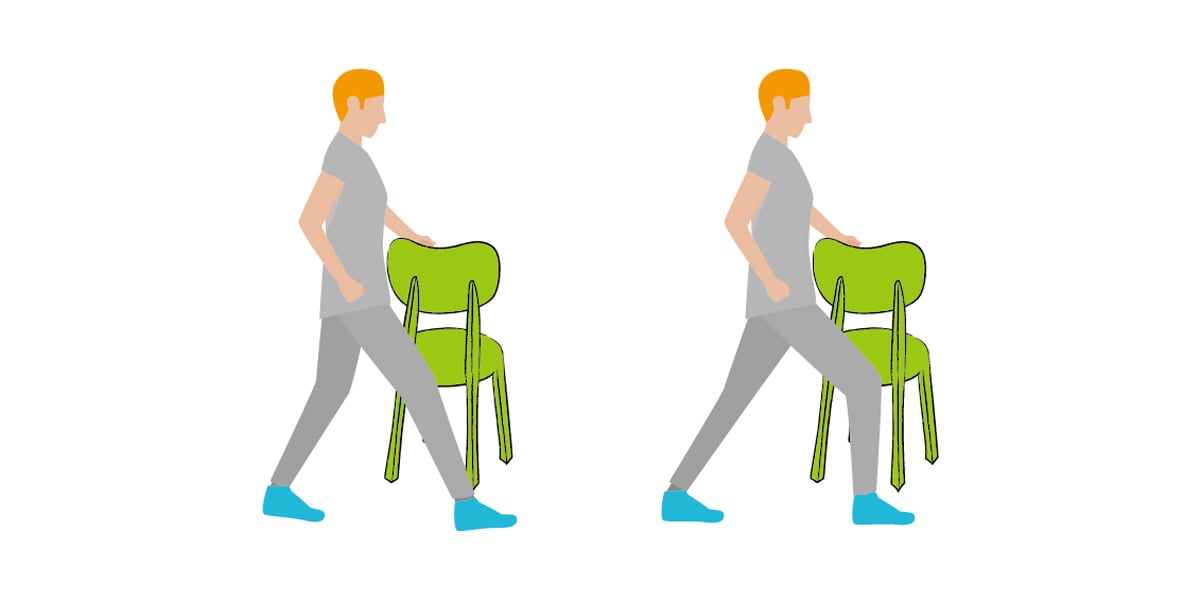
Calf muscle stretch: while doing the stretch, try to maintain the target leg(back leg) straight and you will feel tightness on your calf muscle. Hold the position for 10 seconds, repeat for 5 times and then switch.
Take note, however, that calf muscle stretching should not be painful or excruciating in any way. Instead, it should warm your body up for strengthening exercises.
Research shows that performing daily calf raises decrease plantar fasciitis pain. The inner foot muscles will grow stronger over time, gradually supporting the arch of your foot and becoming able to withstand more weight and improve your daily activities.
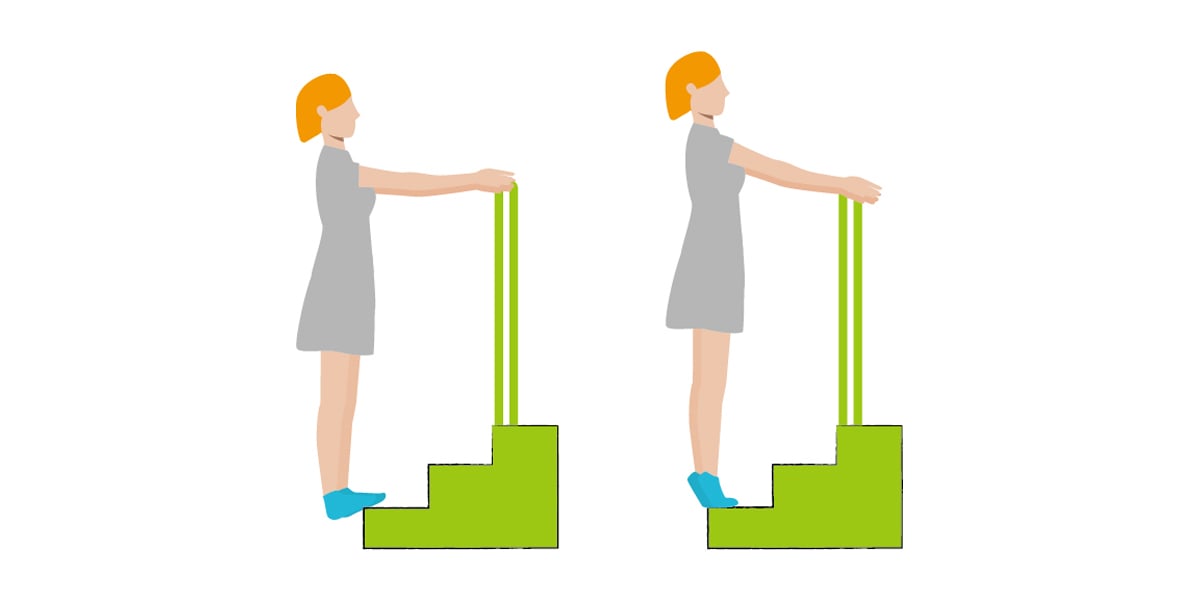
Calf raises and calf strengthening combination with steps: place your 1/3 foot on the step. Sink down and feel tightness on your calf muscle for 10 seconds. And then raise up and squeeze your calf muscle for 10 seconds. Repeat the cycle for 5 times.
As you attend physical therapy, you may be asked to use massage balls, night splints, or heel cups to help ease the pain and reduce pressure.

Heel cups are designed to reduce heel pressure and release your heel pain. Inside the cup, there are gel materials producing soft surface. The heel cups also help to decrease the overstretch the ligament by providing small amount of height.
4. Putting either hot or cold packs.
Research shows evidence that cold therapy reduces inflammation, and many patients have reported that it has helped ease the pain.
During the acute or inflamed stage, take an ice pack and place it on the underside of your foot, leaving it for 15 minutes. To combine this idea with the massage ball, it is also recommended to roll your foot over a frozen bottle of water.
On the other hand, heat therapy increases the blood flow on the applied area, soothing the muscles while speeding up the healing process. Use a hot pack or hot compress for 15-20 minutes, repeating this about 3 to 4 times a day.
Try and see which temperature works best for your body, and use it to decrease pain.
Your doctor may also advise you to take some ibuprofen or naproxen to ease your discomfort. For more painful cases, he or she may also recommend steroid medication.
How the treatment works: Bunions
As a rule of toe, doctors do not recommend surgery until the pain is already unbearable. To prevent that day from happening, there are a few ways you can prevent your bunions from worsening. Here are a few of them:
1. Buying better shoes.
According to Harvard Health Publishing, changing your footwear can greatly decrease bunion pain and prevent it from worsening. It is therefore paramount to know what kind of shoe you need to look for.
The higher the heel, the greater the pressure on your toes. With this in mind, you should look for heels that do not go over two inches. Or, better yet, avoid heels in general and look for shoes that are more comfortable to walk in.
Wider, more flexible soles provide better support, relieving toes of additional pressure. In line with this, the toe box (or the part that surrounds the front of the foot) should be wide enough to accommodate the bunion. This would also prevent blisters or infections that normally happen when bunions continuously hit the inside of your shoe. Also, the heel counter needs to be stable and keep your heel secure while walking.
You may also opt to purchase shoe inserts that will help you position your feet properly. These are usually prescription orthotic devices or over-the-counter arch supports.
Drugstores also offer moleskins or gel-filled pads that can protect your bunion from friction. These are helpful accessories whether you are wearing open-toed sandals or rubber shoes.
2. Maintain a healthy lifestyle.
According to Dr. Bart Gasworth of the University of Chicago, obesity can negatively impact the structure of your foot, placing unnecessary pressure on your joints. By seeing a dietician, following meal plans, and exercising, you can keep your bunion from worsening.
3. Using orthotics.
As with plantar fasciitis, physical therapy and orthotic devices are greatly encouraged for people with bunions. Night splints may help correct bunions and reduce discomfort.
4. Placing hot or cold packs on the bunion.
As with the previous section, placing hot or cold packs is up to your discretion.
Dealing with chronic pain
Experiencing chronic pain in your calves or plantar fascia will not always mean that you have plantar fasciitis or severe valgus big toe. Sometimes, you may just be exhausted from long days at work and have little opportunity to recuperate. This may cause discomfort all day long, preventing you from sleeping well at night.
Heat can relieve muscles, relax the ligament, improve the body's functions, and reduce heaviness. Hot packs help blood vessels dilate, improve blood circulation, help the body's metabolism, promote cell metabolism, and effectively improve the tissues ‘s self-healing ability. It further increases the extensibility of soft tissues and reduces joint stiffness and muscle tightening. And hot compress can also reduce pain, so as to soothe and relax emotions. When done before your daily stretches or exercises, your muscles are no longer tight with friction.
Your feet are an important part of your body and they often go unnoticed. However, when they are in pain, this can definitely affect your mood and impede the normal functions of your whole body.
Additional necessity: A healthy sleeping routine
Getting a healthy amount of sleep starts with planning your sleep routine. Your feet, whether you are sitting or standing, support the weight of your body throughout the day.
If you stretch your calves and place them on a 4D DWF electric foot warmer or heating pad before bed, you will go to bed feeling more relaxed.
Our team at Wellcare BBC(Best Bed Climate) has designed a non-medical electric foot warmer for this purpose, bringing warmth to your extremities. When your feet are warm, the heat circulates throughout your entire body. Our warmers not only relaxes your tendons, but it also increases your likelihood for a good night’s sleep.
If you want to know more about Wellcare 4D DWF electric foot warmer, please click the button below.
We aspire for better health for our readers, liberate them from their painful episodes, and empower them to pursue their goals and aspirations, and future endeavours pain-free.


.png?width=512&name=united-kingdom%20(1).png)

